By Dr. Deepak Mehta, DDS
Introduction
The use of direct composite resin restorations is on the rise due to the esthetic demand of patients. Current composite resin materials are inert. They are bonded to tooth structure by use of adhesives. The weakest link in a composite restoration is the interface between tooth structure and restorative material, where micro gaps trap biofilms leading to secondary caries and post-operative sensitivity.
The recent development of "bioactive" composite resin represents a significant advancement in the field of restorative dentistry. The advantage of these materials is that they serve as a mechanism by which calcium, phosphate & fluoride is released creating a precipitate of hydroxyapatite on the material's surface.
In recent times, manufacturers have aimed at developing materials with better bond strengths and low polymerization shrinkage; however, these materials still remain passive in the oral cavity and are subject to secondary caries. The introduction of bioactive composite resins attempt to inhibit secondary caries and promote remineralization.
This paper presents a case study that outlines the technique to manage a deep carious lesion with placement of Predicta Bulk bioactive restorative material that releases calcium, phosphate, and fluoride to stimulate mineral apatite formation and remineralization at the material-tooth interface.
Case Report
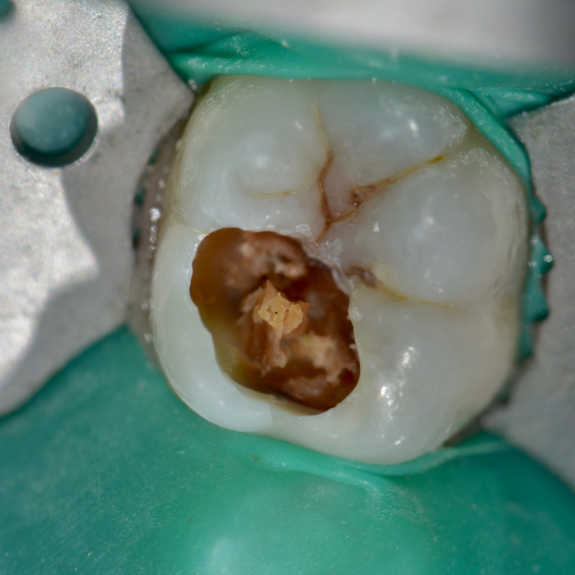
A female patient presented with sensitivity and occasional pain on stimulus in her lower left back tooth. On clinical examination deep carious lesion was present in her lower left first molar tooth (Fig.1). Tooth was non tender to percussion. Radiographic examination revealed deep lesion in close proximity to the pulp with no significant periapical changes (Fig. 2). Patient had a high caries index and therefore a bioactive restoration with Predicta Bulk was considered.



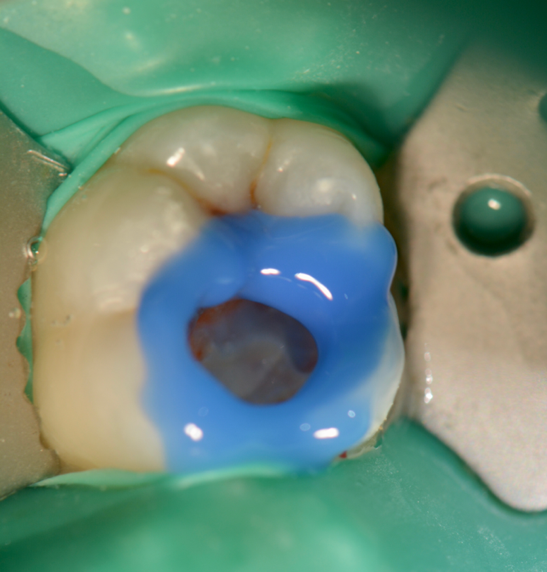
Next, selective etching protocol with phosphoric acid was performed for 20seconds (Fig. 5). Then the preparation was rinsed and gently air-dried. Dentin adhesive (Universal Adhesive, Parkell) was applied that may be used with self-etch, selective-etch (ie, etching only the enamel), and total-etch methods. The adhesive was applied to the preparation using a rubbing motion for 20 seconds keeping the surface moist (Fig 6). A second coat of the adhesive was applied for an additional 20 seconds. Using an air-water syringe, the surface was air-thinned for 10 to 15 seconds to evaporate the solvent. The surfaces were light-cured for 20 seconds.
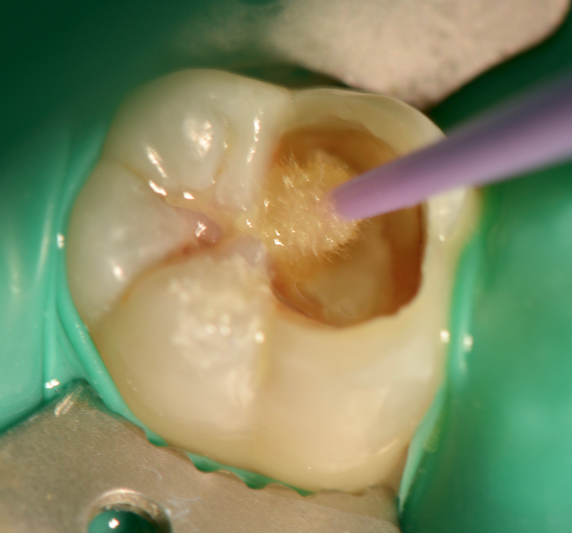
Predicta Bulk composite is available in two different consistencies, high viscosity and low viscosity. A bendable metal-tipped mixing tip, provided by the manufacturer, was used to help facilitate the application of the composite into the deepest portion of the cavity preparation (Figure 7, 8).


Starting from one junction of the box of the cavity preparation, the bioactive bulk composite was injected to fill the entire cavity preparation (Figure 9). Because the restorative material is dual-cure, it is advised to wait at least 1 minute before light-curing the material.
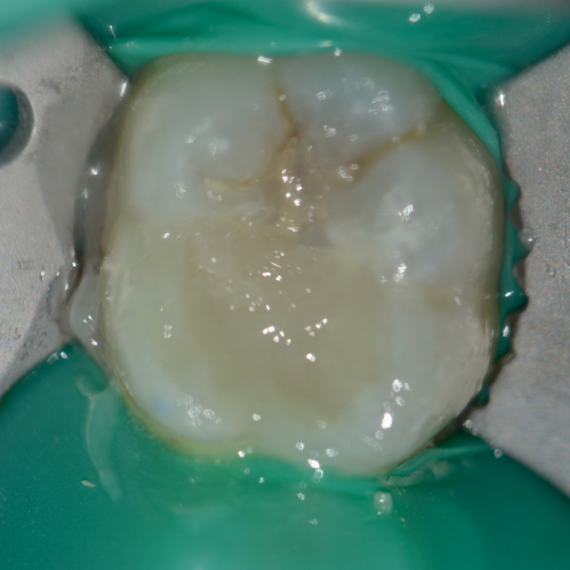

With a series of different finishing burs, the occlusal surface was finished and polished (Figure 10). The occlusion was verified. The occlusal surface was then smoothed with polishers and the restoration was polished with polishing paste. Post-operative radiograph revealed the extent of Predicta due to its excellent radiopacity (Figure 11).

During the follow up period of four months, the restoration showed no unfavorable events. It displayed excellent quality with no marginal failure. No signs of gingival inflammation or increased plaque accumulation was observed. After four months the restoration showed a satisfactory clinical performance considering patient with high caries index (Fig. 12).

Conclusion
Secondary caries is the primary cause of composite resin restoration failure. Dental material science has always evolved to produce newer restorative materials that not only satisfy the esthetic demands of patients but now may play an active role in preventing the cause of failure. Restorative materials that can release calcium, phosphate, and fluoride, creating a precipitate of hydroxyapatite on their surface, no longer are considered inert but become active in the prevention of recurrent marginal failure.

